C O A C H I N G
What even is the thyroid?
Introduction
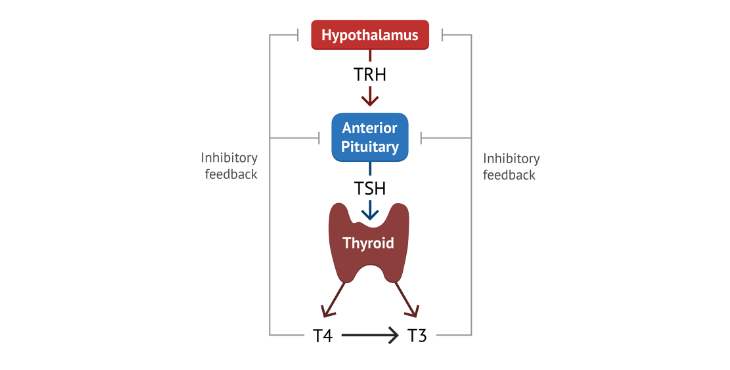
The metabolic and physiologic effects of the thyroid system occur mainly via two hormones, triiodothyronine (T3) and thyroxine (T4). However, these hormones are regulated by a complex system called the hypothalamic-pituitary-thyroid axis. This is a system in which our brain communicates with our pituitary gland, then our pituitary gland will subsequently communicate with our thyroid gland to stimulate the production of T3 and T4. T3 is considered the active thyroid hormone because it is much stronger than T4. However, most of the T3 within the body was actually originally T4, and was simply converted into T3. Today we will break down the production, regulation, and physiological effects of the thyroid hormones, so you have a bit better of an understanding of what the thyroid actually does.
Hypothalamic pituitary axis
The thyroid is a gland, or large group of cells, that sits right under your larynx, oftentimes referred to as your Adam's apple. That said, the production of the thyroid hormone actually begins in a region of your brain referred to as your hypothalamus. The hypothalamus regulates functions such as hunger, body temperature, metabolic rate, urine output, heart rate, blood pressure and other homeostatic functios by modulating the nervous system and the production of different hormones, such as the thyroid hormones.
The hypothalamus does not directly interact with the thyroid gland, rather it interacts with the pituitary gland. The pituitary gland is a small subsection of the brain right below the hypothalamus that is the site for the production of many different hormones. When it comes to the thyroid, after recess signal from the hypothalamus, the pituitary gland with send a signal to the thyroid gland to gather the necessary resources, and begin creating and releasing the thyroid hormones (T3 and T4) into the bloodstream.
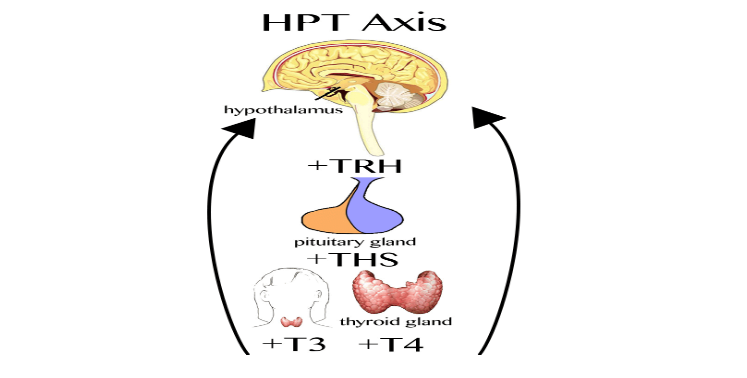
TRH
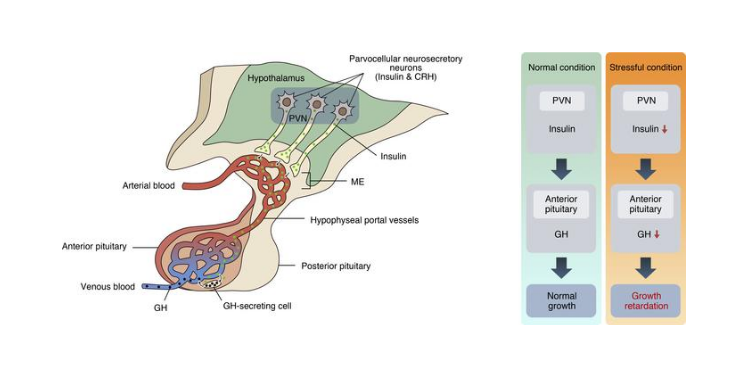
The hypothalamus is made up of a bundle of different neurons. Don't get confused when I say neurons, a neuron is simply the cells within the brain that release neurotransmitters and other chemical messengers. Specifically, in the paraventricular nucleus of the hypothalamus, we release a chemical called thyrotropin releasing hormone (TRH). This chemical is released into the vascular system that connects the hypothalamus with the pituitary gland. TRH binds to the TRH receptor on the thyrotropic cells within the pituitary gland. These are cells that contain the receptor for TRH, and are capable of responding to it by producing the next chemical messenger in this assembly line called thyroid stimulating hormone (TSH).
TSH
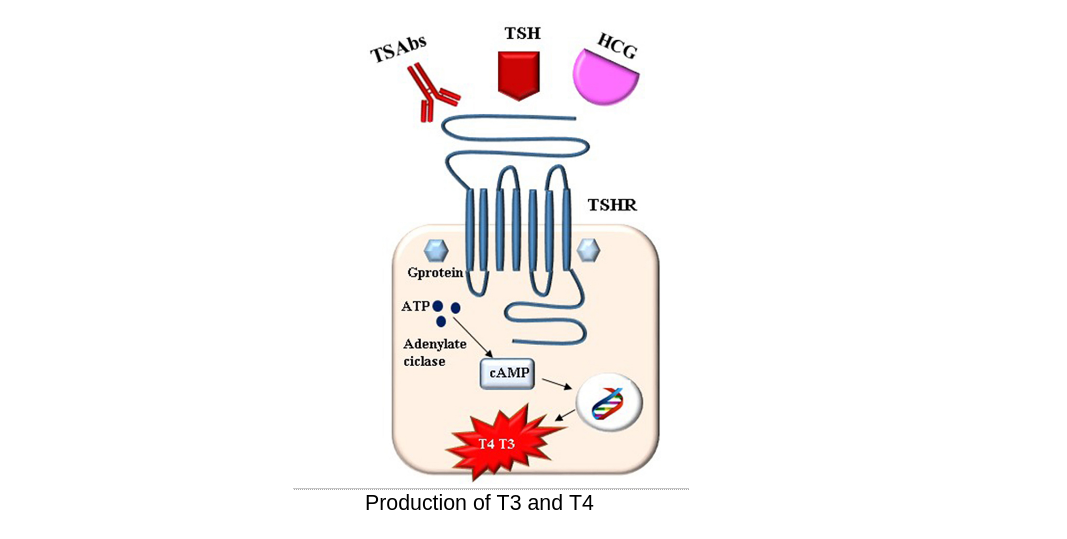
TSH acts very similar to TRH, except it's released from the pituitary gland, and stimulates the thyroid gland to produce and release the thyroid hormones. The TSH receptors are located on the cells located on the exterior of the thyroid gland, referred to as the follicular cells. If you are interested, here is how the TSH- receptor works.
The TSH-receptor is a specific type of receptor called a G-Protein receptor. Simply, the TSH-receptor activates a G-Protein inside of the cell, which interacts with a specific enzyme called adenylyl cyclase. Adenylyl cyclase takes ATP and converts it into cyclic AMP (cAMP).
cAMP interacts with another enzyme called protein kinase A (PKA). PKA transiently modulates thyroid cells to begin producing thyroid hormone. PKA phosphorylates transcription factors within the cell. That is just a fancy way of saying it stimulates specific pieces of DNA within the cell that code for genes related to the production of, in this case, thyroid hormone. In short, PKA causes a cell to start the process of thyroid production.
Production of T3 and T4
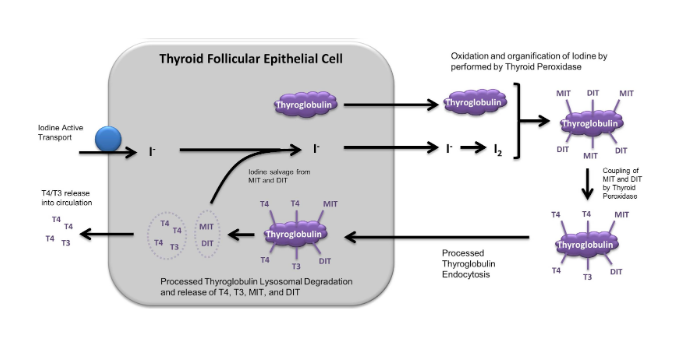
The production of thyroid hormone starts with the production of thyroglobulin, a large protein containing many mocules of tyrosine, the amino acid contained in the active thyroid hormones. TSH stimulates it's release into the interstitial portion of the thyroid gland, the site of thyroid hormone production. The active hormones are made out of two components, iodine and tyrosine. Thyroglobulin is cleaved and used as a source of tyrosine, and the iodine is uptaken out of the bloodstream into the thyroid gland. In the bloodstream, iodine (I) is typically in the form of iodide (I−), meaning it has an additional electron in respect to iodine. Thus, iodide will commonly bind to sodium, and enter into the thyroid cell. There is a protein on the thyroid cell called pendrin, which will pump iodide into the follicular lumen. However, because iodide has an extra electron, it is considered highly reactive and possibly damaging.
No fear, because there is an enzyme in follicular lumen called thyroid peroxidase (TPO) which oxidizes iodide. Oxidation is the process by which an electron is transferred to oxygen, thus iodide loses an electron and forms the much less damaging iodine. That said, TPO has many other functions. TPO then functions to link iodine and links it to the tyrosine molecules within thyroglobulin. If it links 1 iodine it creates monoiodotyrosine (T1), and if it links 2 iodine it will create diiodotyrosine (T2). Just when you thought this enzyme was done, TPO has a third function of combining T1 to a molecule, T2 to make T3, or combining two T2 molecules together to make T4.
Thyroglobulin now has molecules of T3 and T4 contained within it, but we now need to cleave off these molecules and release them into a bloodstream, and leave behind the rest of the large protein to be recycled and reused for further thyroid hormone production. This occurs in the thyroid follicle. The thyroglobulin is taken into the thyroid follicle by endocytosis, and cleaved by proteolytic enzymes. Proteolytic enzymes are enzymes whose main function is to cleave and break down large protein molecules. These enzymes begin cleaving thyroglobulin releasing T3 and T4. It should be noted, it is estimated to be about a 4:1 ratio of T4 to T3, meaning 80% of the thyroid hormone produced is in an inactive form.
Finally, T3 and T4 are released into the bloodstream. T3 and T4 are transported in the bloodstream bound to different carrying proteins, such as thyroxine binding globulin (TBG), thyroxine binding prealbumin (TBPA), or albumin. Thyroid hormones are mainly transported by TBG however (1).
Function of T3 and T4
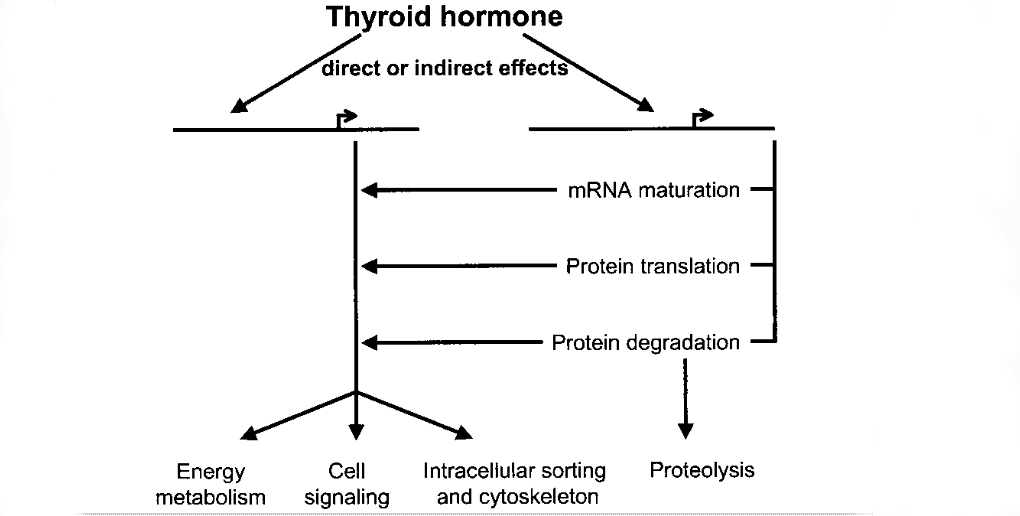
T3 is the hormone that actually exerts physiological functions. T4 can be deiodinated, meaning it loses an iodine, to create the active hormone T3. The thyroid hormone does not have a single location in the body in which it exudes its effects. Rather, thyroid hormones affect almost every cell in the body, but its effects depend on the type of cell it is interacting with. The broad effect of the thyroid hormones is to alter DNA expression. Simply, they can upregulate or downregulate the production of different molecules inside of the cell, which is how these hormones exert their physiological functions. However, the proteins that are upregulated or downregulated or different depending on the location of the cell.
The thyroid receptor
Thyroid hormones are lipid soluble, meaning they can simply enter into the cell without the need for a membrane transporter. When in the cell the thyroid hormone binds to the thyroid receptor, which creates what is referred to as a complex. This complex then interacts with proteins inside the cell called thyroid response elements (TRE) which are proteins that can bind to the DNA and alter the expression of different proteins.
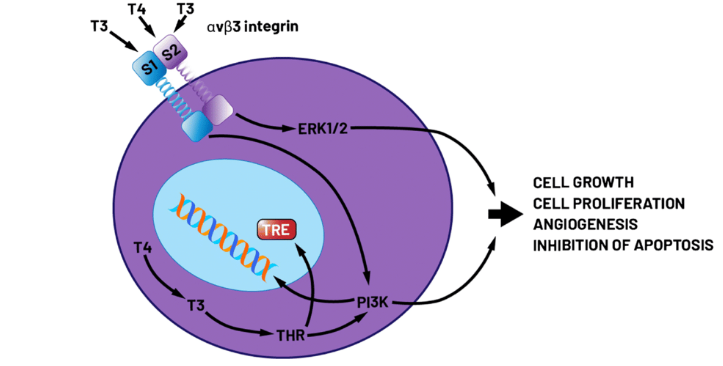
With that being said, let's look at some of the genetic expressions modulated by thyroid hormone.
METABOLISM
The thyroid hormone can drastically alter one's resting metabolic rate. It's estimated that the concentration of thyroid hormone could as much as double one's resting metabolic rate in the presence of too much thyroid hormone, and reduce one's resting metabolic rate by as much as 50% when deficient in the hormone (2). Through a myriad of different proteins, one of the best understood and most obvious effects of the thyroid is to increase one's resting metabolic rate. Thyroid hormones act mainly on the muscles and the fat cells to increase the production and usage of ATP. To make sure this discussion makes sense, it's important to understand ATP. The human body turns the food that we eat into a chemical called ATP. This ATP is used as energy to power almost every single physiological function and reaction within the body. The more ATP we require, the higher our metabolic rate. The more ATP we create, the more fuels, such as fatty acids, amino acids and glucose, we will break down in order to maintain enough ATP for the cell. Thyroid increases the production of ATP by altering genes that subsequently increase the production , size, and efficiency of the mitochondria within our cells. The mitochondria are the organelles in the cell responsible for the production of ATP. The more abundant and efficient they are, the more ATP we can and will produce. Additionally, there is an increase in the production of the proteins involved in breaking down fatty acids, glucose, and amino acids in order for them to be turned into energy. These are referred to as respiratory chain proteins. Finally, there is an increase in the production of different cellular protein channels that use ATP in order to function, thus increasing the cell usage of ATP.
Individuals with excess thyroid hormone will have a very fast metabolic rate, making is difficult to put on body weight. Conversely individuals with a deficiency in thyroid hormone will typically put on body fat despite having a seemingly low caloric intake.
Additionally, due to the lack of ATP, individuals with low thyroid are often hypoactive, meaning they are very low on energy. Individuals with high thyroid typically are hyperactive and appear to have an abundance, sometimes excess, of energy.
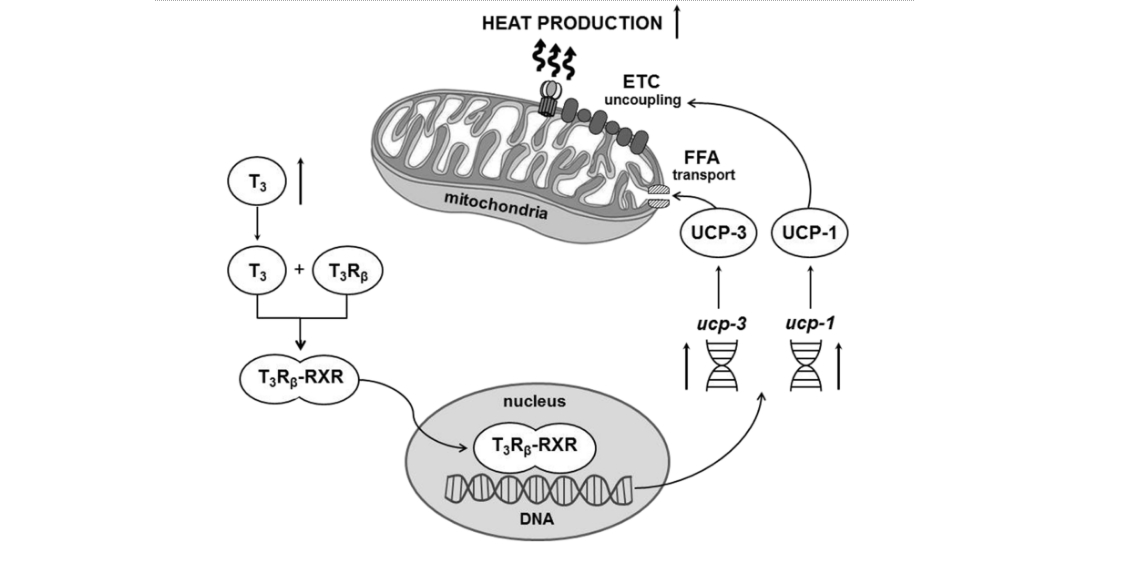
Uncoupling
The thyroid hormone also increases the production of uncoupling proteins. Uncoupling is a phenomenon in which during the process of producing atp, the cell releases some of the energy as heat into the environment rather than turning it into ATP. This occurs via proteins that are embedded in the mitochondria referred to as uncoupling proteins. The more of these proteins within our mitochondria, the more stored energy we need to break down in order to produce the same amount of ATP because the percentage of our substrate is being converted to heat rather than ATP.. This uncoupling effect is one reason why in a state of excess thyroid hormone, individuals are extremely hot and oftentimes sweat excessively. Conversely, in a state of deficiency, individuals often get cold easily, and have lower waking body temperature (3).
Breakdown and release of stored energy
The thyroid hormone increases the amount of circulating glucose, fatty acids, and amino acids in our bloodstream. It does this through a few mechanisms. The thyroid hormone increases lipolysis, or the breakdown of fatty acids from the adipose tissue. It also increases glycogenolysis, or the breakdown of stored glucose from the liver, which is then released into the bloodstream. There is also an increase is proteolysis, or the breakdown of proteins typically from the skeletal muscle. And finally, the thyroid hormone increases gluconeogenesis and lipogenesis in the liver, which is the creation of glucose and fatty acids in the liver. The substrate for gluconeogenesis and lipogenesis are typically things such as glycerol, Amino acids, and lactate. Individuals with excessive thyroid typically have elevated blood glucose. Individuals with low thyroid may also suffer with high blood glucose fatty acids and amino acids. Individuals with a low thyroid may also show high circulating glucose and fatty acids, but this is due to an insufficient uptake of these fuels at the level of the cell, not necessarily due to excess gluconeogenesis of lypogenesis.
Protein turnover
The thyroid hormone has very interesting and conflicting effects in proteins. The thyroid hormone stimulates both the catabolism of proteins, and the synthesis of proteins. This is referred to as protein turnover, or the process of breaking down old proteins and building up new ones. These include the proteins that make up the skin, hair, nails, bones, and skeletal muscle.
Individuals with low thyroid oftentimes have hair loss, brittle nails, lower bone mass and dry skin, due to insufficient protein turnover and regeneration. Additionally they typically have lower muscle mass due to decreased rates of protein synthesis. With that said, individuals with high thyroid typically do not suffer with hair skin and nail issues, however they do often suffer from excessive protein catabolism due to exceedingly high energy demands. Thus, they also are characterized by a difficulty putting on muscle mass (4).
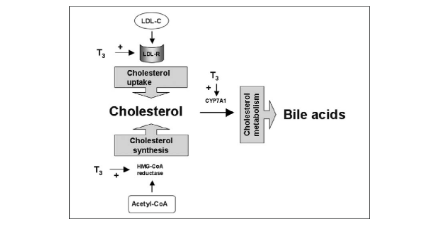
Cholesterol metabolism
Another pathway by which the thyroid hormone has contrasting affects is on the production of cholesterol, and the uptake of cholesterol carrying Lipoproteins (HDL and LDL) out of the bloodstream. The thyroid hormones stimulate the production of cholesterol in the liver, and creation and release of Lipoproteins carrying this cholesterol. However, the thyroid hormone also increases the presence of LDL receptors around the body, and specifically on the liver. Thus, the thyroid hormone is extremely important for proper cholesterol transport around the body using Lipo proteins. For more information about cholesterol transport and the function of these Lipoproteins, I will release a future article all about cholesterol.
Individuals with excess thyroid hormones appear to have hypocholesterolemia, meaning low levels of cholesterol in the blood, because the uptake of these Lipoproteins exceeds the production of them. Conversely, individuals with low thyroids typically have elevated LDL and HDL cholesterol. Importantly an elevated HDL in tandem with a high LDL is a blood work result that is very telling of a low thyroid, as many individuals with high LDL typically have lower HDL (5).
Heart rate and blood pressure
One of the proteins regulated by thyroid hormone is the beta 1 adrenergic receptor. These receptors are predominantly found on the heart, and fat tissue. This is the receptor mainly for adrenaline. On the fat tissue, stimulation of this receptor increases lipolysis, which is the breakdown and release of fatty acids into the bloodstream. In the heart, stimulation of these receptors increase heart rate and stroke volume, thus increasing blood pressure along with heart rate. Individuals with excess thyroid may have excessively high heart rate and blood pressure, whereas individuals with low thyroid or characterized by having low blood pressure and a low heart rate (1).
Gastric emptying
Interestingly the thyroid hormones stimulate gastric emptying, or the movement of food through the digestive system and into the stool. The more thyroid hormone one has, the quicker your gastric emptying rate will typically be. Thus, individuals with high thyroid typically have symptoms of diarrhea and Malabsorption, due to excessively quick gastric emptying. Individuals with low thyroid frequently report constipation and excessive bloating due to slow low Benton of food through the digestive system and prolonged gastric emptying (6).
Brain development
It appears the thyroid hormone has exceptionally vast rolls within fetal development. This includes proper development of the brain, photoreceptors of the eye, and proper formation of the auditory system. This is likely due to its role in protein turnover, because one of the most important processes that occurs during fetal development is actually the loss of unwanted neural connections, referred to as synaptic pruning. Babies who have genetic hypothyroid states typically have perturbed and disrupted development both physically and cognitively (7).
Negative feedback
The thyroid hormones typically work through a negative feedback loop. In essence, the thyroid hormones are able to inhibit the TRH neurons within the hypothalamus, and the TSH-producing cells within the pituitary gland. Thus, the thyroid gland no longer gets the signal from the hypothalamic adrenal axis to continue to produce active thyroid hormones. This is referred to as end product inhibition, in which the end product, in this case the thyroid hormones, is able to inhibit its own production via inhibiting the initial stimulus sent from the brain and the pituitary gland. This will be extremely important in the next section, in which we will discuss using blood work to understand the state of one's thyroid, and what could be causing both hypothyroid ir hyperthyroid states (1).
Thyroid testing
With a simple blood draw, one can get levels of t3, t4, tsh, reverse t3, and thyroid antibodies. There are a few different phenotypes (results) that may raise suspicion that an individual's thyroid may be over or under performing.
Reverse T3
As mentioned, people can be converted into t3. However, T4 can also be converted into the first t3, an inactive form of thyroid. The production of reverse T3 rather than T3 appears to be increased in scenarios of stress, caloric restriction, selenium deficiency, heavy metal toxicity, and sickness. The exact mechanism behind this isn't yet fully understood, but if an individual has normal levels of TSH, or even high TSH, with low levels of T3 and high levels of reverse T3, these are the physiological parameters that may be causing it.
TSH
Elevated TSH typically means the brain desires more thyroid hormone, but the thyroid gland is not producing sufficient amounts of the hormone. High TSH and low thyroid is likely due to a disruption within the pathway of thyroid hormone production within the thyroid gland. However high TSH and high thyroid indicate The brain is somehow not receiving the negative feedback of elevated thyroid hormones.
A high TSH along with high reverse T3 indicate there is excessive conversion of T4 into reverse T3 rather than the active form of T3.
Very low TSH and high T3 Indicates that an individual is likely in a high thyroid state, in which their thyroid gland is producing excessive amounts of thyroid hormones, despite lack of stimulation from the pituitary gland. This could be caused by a myriad of different things, such as some sort of thyroid tumor.
Low TSH along with low T3 indicate some sort of issue within the initial hypothalamic pituitary access.
T3
T3 is likely going to provide you the most accurate picture of someone's thyroid activity, and will typically match up the best with their symptoms. Elevated T3 almost always indicates some degree of hyperthyroid state, but could also indicate some sort of resistance to thyroid if an individual has symptoms of low or normal thyroid. Low T3 almost always correlates with symptoms of low thyroid as discussed above.
Importantly, high T3 in the presence of high TSH typically indicates a a hyperthyroid state being driven by an inadequate inhibitin of the pituitary signaling that should occur in a state of high T3. However elevated T3 in the presence of low or normal TSH indicates hyperthyroid that is being driven by the thyroid gland itself.
Low T3 in the presence of low TSH indicates hypothyroid being driven by the hypothalamus or pituitary gland. Low T3 in the presence of normal or high TSH indicates hypothyroid that is being driven by an inadequate production of thyroid hormones in the thyroid gland, or excessive production of reverse T3.
T4
T4 is not as indicative as T3 , but it could be useful. High levels of T4 in the presence of normal TSH and low T3 indicate an impaired ability to convert T4 into T3, however this is quite rare. High levels of T4 in the presence of high T3 typically occur in hypothyroid individuals. High levels of T4 in the presence of low normal T3 probably do not necessarily indicate any sort of physiological impairment.
Low levels of T4 in the presence of low T3 indicate a hypothyroid state, in which you would likely need to look at all the other markers in order to make an adequate assessment as to what is causing this state.
Thyroid antibodies
On blood work, one can get thyroid antibodies tested. If elevated, this indicates the individual is having some sort of autoimmune response to their thyroid gland, which will likely lead to improper functioning of the thyroid complex as a whole.
Cheap at home testing
In addition to the indicators I listed above, one of the easiest and cheapest ways to ascertain an individual's thyroid status is taking a body temperature measurement in the morning. If the body temperature is lower than 96.5, it may indicate a decreased thyroid activity. If it is above 98.5, it might be indicative of excess thyroid, given they also have some of the other symptoms.
Impact of nutrition and lifestyle on the thyroid
There are a few very critical micronutrients and other nutritional factors that play a role in proper thyroid function. A deficiency in micronutrients specifically zinc copper, selenium, iodine, or sodium may negatively impactful thyroid and lead to a low fthyroud state. However, many other micronutrients can interplay with the thyroid and cause a low thyroid condition. Additionally, an excess of heavy metals can inhibit, impair, and/or damage the thyroid, and could also lead to impairments in proper thyroid function.
Moreover, because the thyroid hormones do require tyrosine which is an Amino acid,
A dietary inadequacy in protein could drive low thyroid production.
That said, a caloric deficit can lead to a significant and noticeable decline in a production of the active thyroid hormones, which can be mediated by decreased signaling from the brain or pituitary gland, decreased production of thyroid hormones, or excessive conversion of T4 into t3. However, a high protein diet appears to be able to mitigate metabolic slow down during an acute or prolonged caloric deficit.
The very last thing I will mention is that it doesn't appear that excessive stress can lower thyroid activity. Stress caused by excessive physical or mental stress, or an underlying illness, sickness, disease, or a mixture of all of these can decrease the production of the active thyroid hormones.
Synopsis
I hope this paper made a few things extremely evident about the thyroid. The first is that it regulates a multitude of different physiological functions, some of which most people don't think about when speaking about the thyroid. Additionally, the regulation of thyroid activity, specifically the production of active thyroid hormones, can be extremely complex, nuanced, and difficult to understand. Thus, while there are many different physiological indicators that an individual may have excessive or deficient levels of thyroid, the best way to ascertain where an individual's thyroid health is, and what might be causing a deficiency or excess, is going to be to get a comprehensive blood analysis. As always I recommended consulting with a doctor before making any conclusions or changes. However, I hope this article at least provided you with insight into the thyroid, and possibly provides you with the background information upon which you can begin to understand your ownl thyroid health using the physical signs and symptoms mentioned earlier, and through the proper interpretation of blood work. But as always, if you have any questions, always feel free to reach out to me!
Citations
https://www.ncbi.nlm.nih.gov/books/NBK500006/ https://www.ncbi.nlm.nih.gov/books/NBK28/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6287687/#:~:text=The%20thyroid%20hormone%20triiodothyronine%20(T,autonomous%20effects%20on%20BAT%20mitochondria. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6403129/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6129606/#:~:text=Thyroid%20dysfunction%2C%20manifesting%20as%20either,disease%20and%2C%20potentially%2C%20mortality. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2833301/ https://www.ncbi.nlm.nih.gov/books/NBK285549/#:~:text=Thyroid%20hormones%20are%20essential%20for,migration%2C%20synaptogenesis%2C%20and%20myelination.